Abstract
INTRODUCTION: While novel agents are being explored as initial treatment (tx) of adults with ALL, cytotoxic chemotherapy remains a standard, particularly for Philadelphia chromosome (Ph)- disease. HyperCVAD is commonly used but has significant toxicity and requires sufficient resources and expertise, especially in older patients (pts). A single-arm phase II trial evaluating dose-adjusted (DA-)EPOCH for adults with ALL demonstrated efficacy and modest toxicity. Here, we compared these outcomes with a retrospective cohort of pts meeting eligibility criteria for the DA-EPOCH trial but received off-study HyperCVAD.
METHODS: Details of the DA-EPOCH study have been reported (ASH 2018, #1519; NCT03023046). Records from pts age > 18 years (yrs) with ALL who received first-line tx with HyperCVAD from Dec 2010 to Jan 2021 were reviewed. Remaining eligibility criteria mirrored the DA-EPOCH study: notably adequate kidney and liver function, ECOG ≤ 2 unless due to ALL, no isolated extramedullary disease, and ineligible for pediatric-inspired tx (ie, Ph- and age 18-39). Pts with Ph+ disease received dasatinib or imatinib (TKI), and rituximab was added for CD20+ disease at physician discretion. Tx consisted of ≤ 8 cycles followed by maintenance (POMP ± TKI) or allogeneic transplant (HCT). Cytogenetic risk was assigned per NCCN. Response was determined by multiparameter flow cytometry of marrow aspirate [measurable residual disease (MRD)- < 0.01% of nucleated mononuclear cells]. Adverse events (AEs) were defined by CTCAE v5.0. Proportions were compared by chi square test and means analyzed by two-tailed t-test.
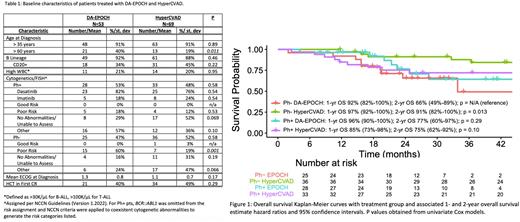
RESULTS: Significantly more pts aged > 60 yrs and with poor-risk cytogenetics received DA-EPOCH; other baseline characteristics were similar (Table 1). In Ph+ treated with hyperCVAD + TKI, 32 (97%) achieved complete remission (CR) after 1 cycle (C1) and 26 (79%) were MRD- within 4 cycles (≤ C4) vs 26 (93%) achieved CR after C1 and 20 (71%) were MRD- ≤ C4 from DA-EPOCH + TKI (p = 0.46 and 0.51, respectively). For Ph- given hyperCVAD, 30 (83%) achieved CR after C1 and 26 (72%) were MRD- ≤ C4, while 18 (72%) achieved CR after C1 and 16 (64%) were MRD- ≤ C4 from DA-EPOCH (p = 0.29 and 0.50, respectively).
Overall survival (OS) is shown in Figure 1. For Ph-, 3-yr EFS estimate was 61% for HyperCVAD vs 33% for DA-EPOCH, and median EFS was not reached vs 15 months (mo), respectively. For Ph+ (with TKI), 3-yr EFS estimate was 51% for HyperCVAD vs 35% for DA-EPOCH, and median EFS was 42 mo vs 15 mo (respectively). In Cox models for EFS with DA-EPOCH for Ph- as the reference, these hazard ratios (HR) and 95% confidence intervals were observed: HyperCVAD for Ph-, HR 0.47 (0.23-0.95, p = 0.036); DA-EPOCH + TKI for Ph+, HR 0.94 (0.48-1.9, p = 0.87); and HyperCVAD + TKI for Ph+, HR 0.67 (0.34-1.3, p = 0.25). In univariate models including all pts, high WBC (>30K/µL for B-ALL and >100K/µL for T-ALL) was associated with not achieving MRD- (p = 0.047) and EFS (p = 0.013) but not mortality; no other factors analyzed had significant associations with these outcomes.
Interaction tests were used to identify factors responsible for differences in MRD-, EFS, and mortality between DA-EPOCH and HyperCVAD. After adjusting for ECOG, poor-risk cytogenetics, WBC, age, and HCT in first CR, the interaction from Ph status yielded p = 0.06 for mortality, suggesting differences in mortality that were observed between regimens varied on Ph status. In a Cox model adjusted for age, mortality was significantly reduced with HyperCVAD for Ph- (HR 0.18, p = 0.005) but not for Ph+ (HR 1.0, p = 0.99).
As for toxicity, significantly more pts given HyperCVAD experienced Grade 4 or 5 AEs (20%) vs DA-EPOCH (6%; p = 0.021). Mean RBC and platelet (plt) transfusions per cycle were higher in those that received HyperCVAD [RBC = 3.3 (standard deviation [SD] 1.4), plt 1.9 (SD 1.5)] than DA-EPOCH [RBC 0.6 (SD 0.7), plt 0.2 (SD 0.5)] (p <0.001 for both). Treatment was stopped early due to cumulative toxicity in 10 pts (14%) given HyperCVAD and 4 (8%) given DA-EPOCH (p = 0.23).
CONCLUSIONS: In our cohorts, more pts given DA-EPOCH had high risk features. DA-EPOCH and HyperCVAD yielded similar outcomes for Ph+ ALL while OS and EFS favored HyperCVAD for Ph- ALL. However, HyperCVAD caused significantly more life-threatening toxicity and reliance on transfusions. These data generally support the use of HyperCVAD over DA-EPOCH yet highlight a role for DA-EPOCH when more intense therapy is not feasible.
Disclosures
Percival:Trillium: Research Funding; Oscotec: Research Funding; Pfizer: Research Funding; Cardiff Oncology: Research Funding; Glycomimetics: Research Funding; Biosight: Research Funding; Celgene/BMS: Research Funding; Abbvie: Research Funding; Ascentage: Research Funding; Telios: Research Funding. Halpern:Bayer Pharmaceuticals: Research Funding; Tolero Pharmaceuticals: Research Funding; Novartis: Research Funding; Imago Biosciences: Research Funding; Gilead Sciences: Research Funding; Jazz Pharmaceuticals: Research Funding; Incyte Pharmaceuticals: Research Funding; Karyopharm Therapeutics: Research Funding; Abbvie: Consultancy; Notable Labs: Consultancy. Ghiuzeli:Sangamo therapeutics: Current equity holder in private company; TG Therapeutics: Current equity holder in private company; Axson therapeutics: Current equity holder in private company; Sorrento therapeutics: Current equity holder in private company; Sorrento therapeutics: Current equity holder in private company; Uniqure: Current equity holder in private company; Repare therapeutics: Current equity holder in private company; Crisp: Current equity holder in private company; Intellia: Current equity holder in private company; Seattle Genetics: Current equity holder in private company. Becker:Notable labs: Research Funding; Glycomimetics: Research Funding; Pfizer Pharmaceuticals: Research Funding; Accordant Health Services (CVS Caremark): Consultancy. Oehler:Novartis: Consultancy; Pfizer, Inc: Consultancy, Research Funding. Orozco:Actinium Pharmaceuticals, Inc.: Other: Site PI for clinical trial(s) sponsored by Actinium and Research Funding. Walter:Janssen Global Services, LLC: Consultancy; Janssen Research and Development: Research Funding; Celgene, Inc: Consultancy, Research Funding; Bristol Myers Squibb, Inc: Consultancy; Kronos Bio, Inc: Consultancy; Jazz Pharmaceuticals: Consultancy, Research Funding; Kite Pharma, Inc: Consultancy; ImmunoGen: Research Funding; BioLineRx, LTd: Consultancy, Research Funding; AbbVie: Consultancy; Selvita: Research Funding; GSK: Consultancy; MacroGenics: Consultancy, Research Funding; New Link Genetics: Consultancy; Pfizer, Inc: Consultancy, Research Funding; Race Oncology LTD: Consultancy; Stemline Therapeutics: Research Funding; Agios: Consultancy, Research Funding; Amgen: Consultancy, Research Funding; Amphivena Therapeutics, Inc: Current equity holder in publicly-traded company; Aptevo Therapeutics: Consultancy, Research Funding; Kura Oncology: Consultancy, Research Funding; Genentech: Consultancy; BerGenBio, ASA: Consultancy; Orum Therapeutics, Inc.: Consultancy; Arog Pharmaceuticals: Research Funding; Astellas Pharma US, Inc: Consultancy; Boston Biomedical, Inc: Consultancy. Estey:Bayer Pharmaceuticals: Research Funding. Cassaday:Merck: Research Funding; Servier: Research Funding; Vanda: Research Funding; Pepromene Bio: Membership on an entity's Board of Directors or advisory committees; Autolus: Membership on an entity's Board of Directors or advisory committees; Kite, a Gilead Company: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Amgen: Consultancy, Research Funding; Seagen: Current Employment, Current equity holder in private company, Other: Spouse employment with Seagen; stock or other ownership in Seagen.; Jazz: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal